Do you work in the medical field?
If yes, then you already know all about SOAP notes.
Whether you are a nurse or doctor, you will have to maintain a Subjective, Objective, Assessment and Plan Note, aka the SOAP note.
So, how to write and maintain this document?
Learn all about it with a SOAP note example!
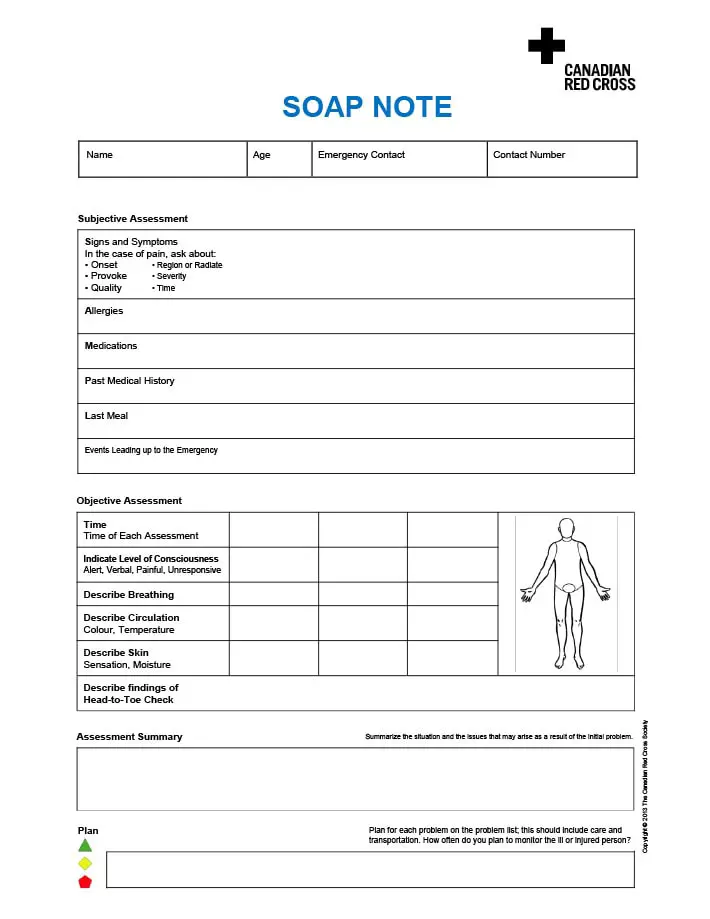
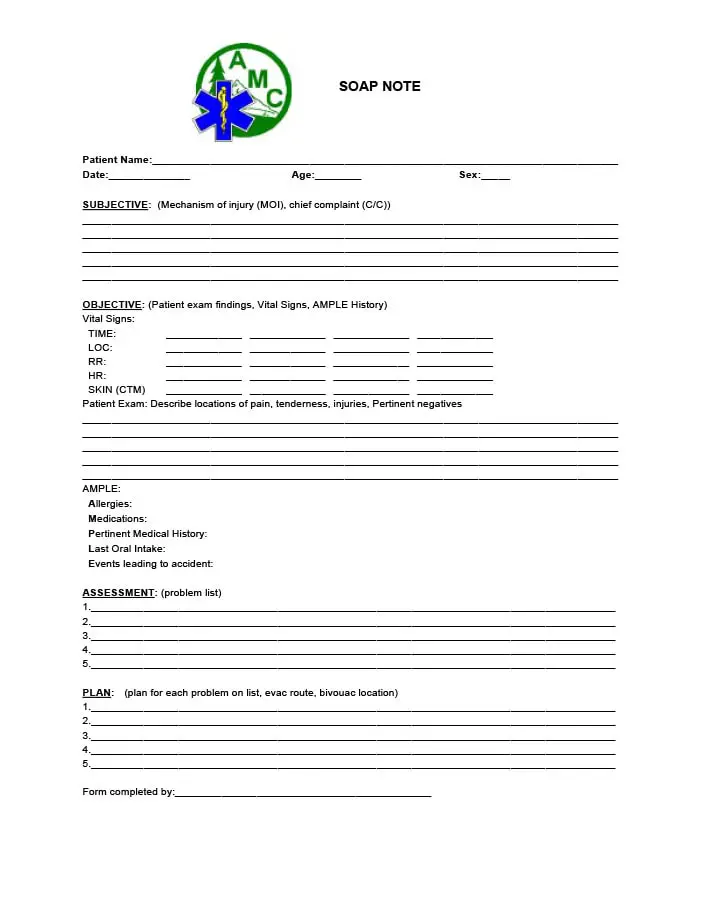
Printable & Editable SOAP Note Examples & Templates in Word, PDF & Excel
As a nurse or physician, you will come across a host of different scenarios during your professional course.
However, despite the significant progress in healthcare software and systems, you cannot skip SOAP notes.
These are vital documentation that every medical attendant needs to maintain.
Well, to save you from trouble, we bring you a free set of vital SOAP note templates. You can download or refer to the SOAP notes to seamlessly use, as and when required.
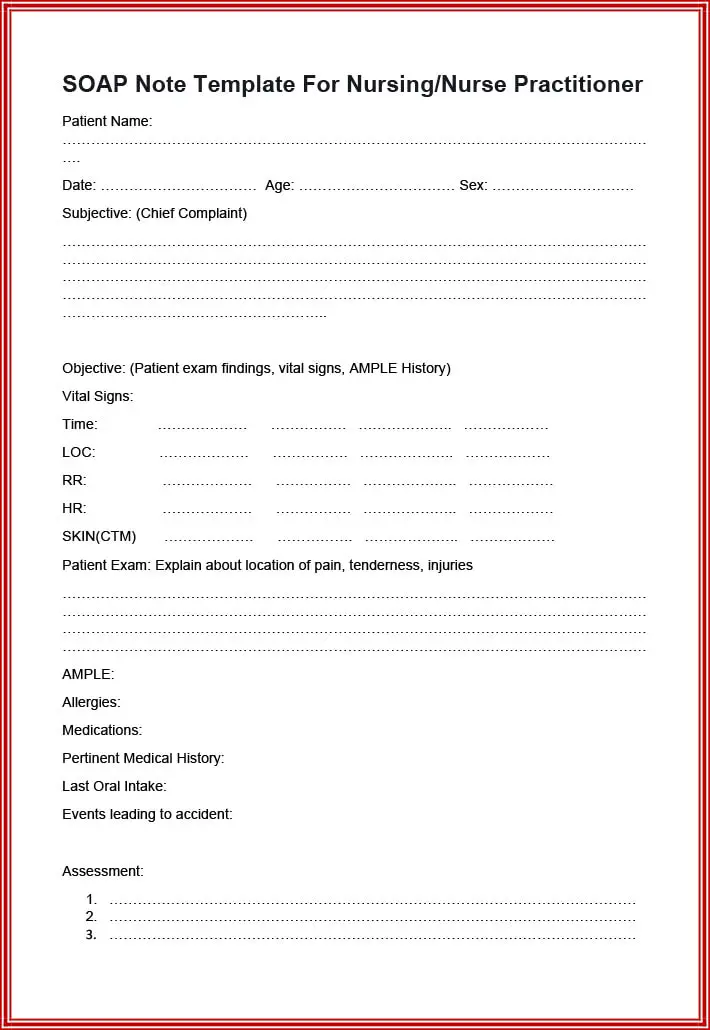
For Nursing/Nurse Practitioners
When you are a nurse or a practitioner, you will face a plethora of different medical scenarios. These can range from common cold and flu to severe diabetes, surgery, and other health disorders.
Here are three examples of patients that you may frequently encounter.
For Cough and Congestion
You must start by writing the subjective section that includes the chief complaint, i.e., cough and congestion.
Next, mention aspects like the thickness and color of phlegm, body ache, and other symptoms. Note each aspect expressed by the patient, like current pain, feelings, medication taken (if any), duration, etc.
It is the most vital section as it will help the other practitioner gain knowledge about the patient’s initial health state.
Remember to also thoroughly note the patient’s medical history, including any related or non-related disorders.
Next, you will need to document the crucial signs, test, physical examination results, etc., in the objective section. For example, blood pressure, temperature, swellings, sinus, chest, abdomen situation, etc.
The last section will be the assessment plan and treatment plan wherein you conclude by suggesting a further treatment, medication, etc. You can mention chest x-ray, medical doses, etc.
For Post Surgery
This example explains how you can write it for an old or existing patient.
Start by mentioning the pain, symptoms, and discomfort condition (if any) in the subjective section. You can then specify the patient’s body movement details, whether s/he has been moved out of bed along with the current diet.
In the objective section, write about the vitals (temperature, pulse, blood pressure, etc.), activity, skin, pain, and abdomen conditions. Also, you need to mention the test and lab results here.
The third section will be your assessment or analysis, for example, the risk of infections due to the XYZ cause.
Lastly, draw out the treatment program to encourage the patient to relax, administer medication, and continue careful monitoring.
For Diabetes Patient
A diabetic patient usually has a long history, and you can opt to go through the medical history forms for accurate specifications.
According to the previous doctor’s note and the current information that the patient communicates, you can create the subjective section.
As you can see in the given example, you will write about the subject’s weight, blood pressure, sugar levels, pains, etc.
Also, mention the medications and allergies, if any.
Followed by this, make sure to notify all the vital signs, glucose levels, and test results, including lungs, heart, abdomen, skin, etc.
In the assessment and plan segment, write your examination report, like the response to treatment and any consultations.
Additionally, mention relevant information on dyslipidemia, hypertension, hernia, and other treatment histories.
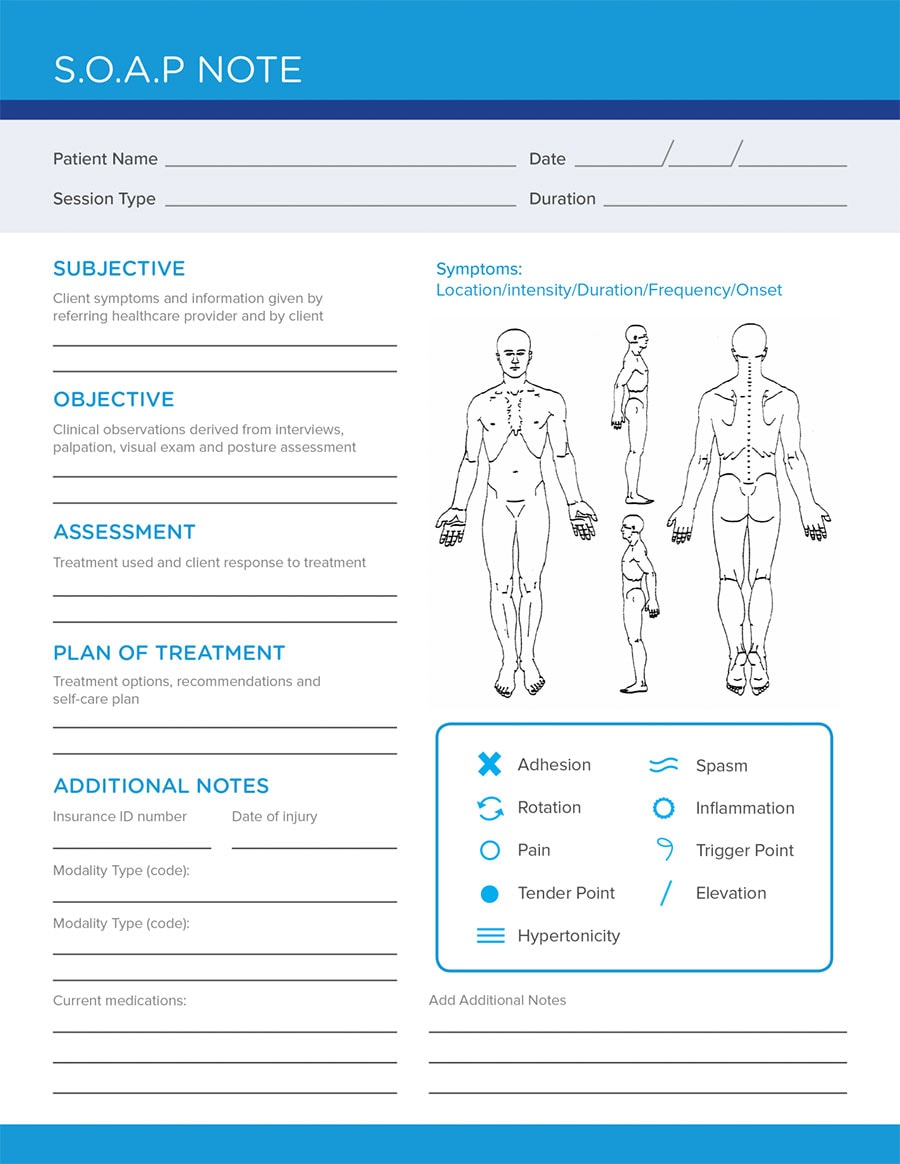
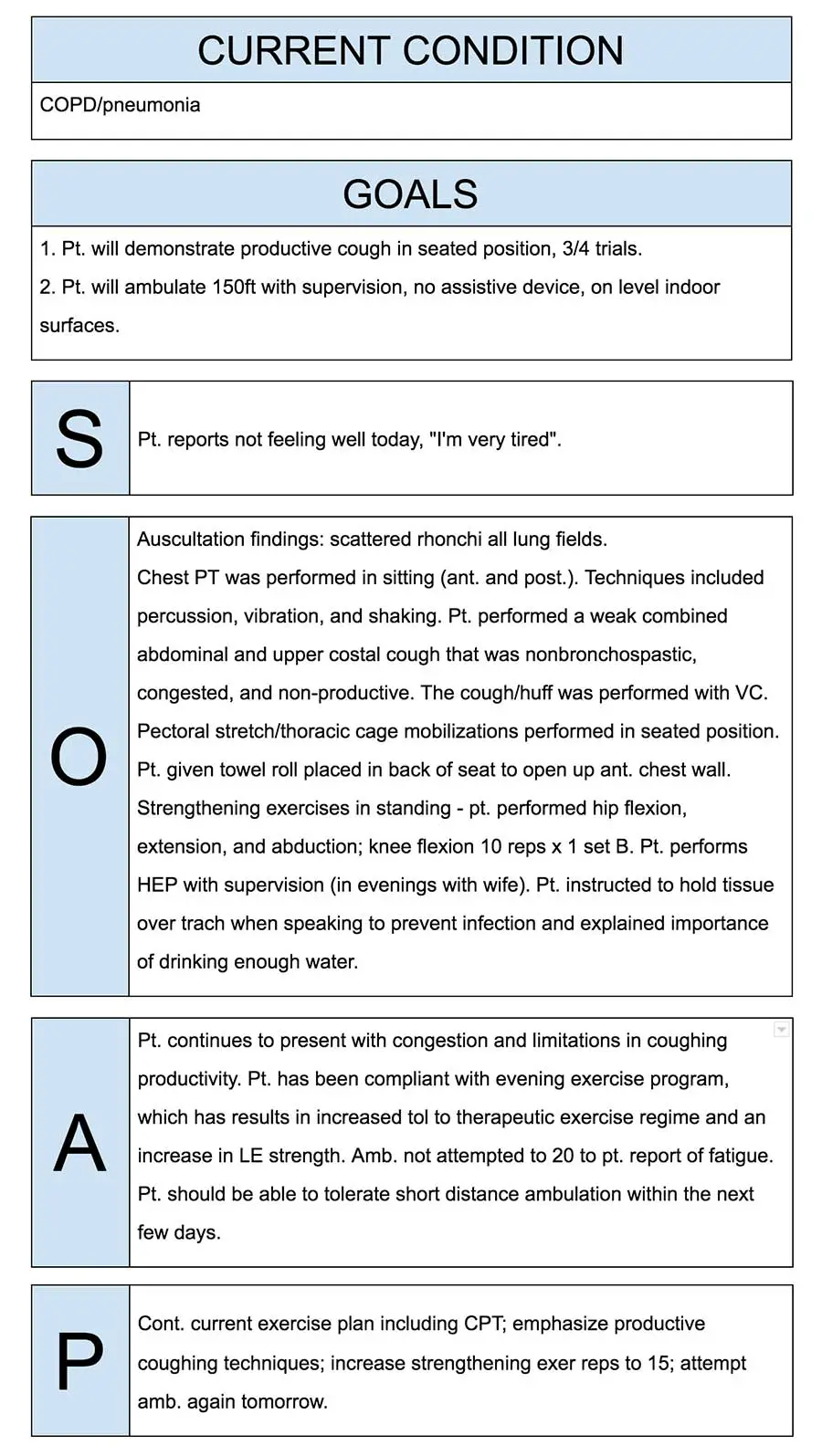
For Physical Therapy
This system introduced by Dr. Lawrence Weed is vital for a physical therapist. More so because such a treatment process usually goes a long way, and during this course, a patient may consult several physicians.
Even the American Physical Therapy Association offers detailed guidelines for the Physical Therapy SOAP notes. Here is a quick overview:
- Types of equipment used for treatment
- Patient’s self-report
- Intervention details
- Subject’s present health status
- Progress in the physical condition
- Complications during the treatment course (if any)
- Details collected from other care providers and the patient’s family
Here is a detailed SOAP Note example for your reference.
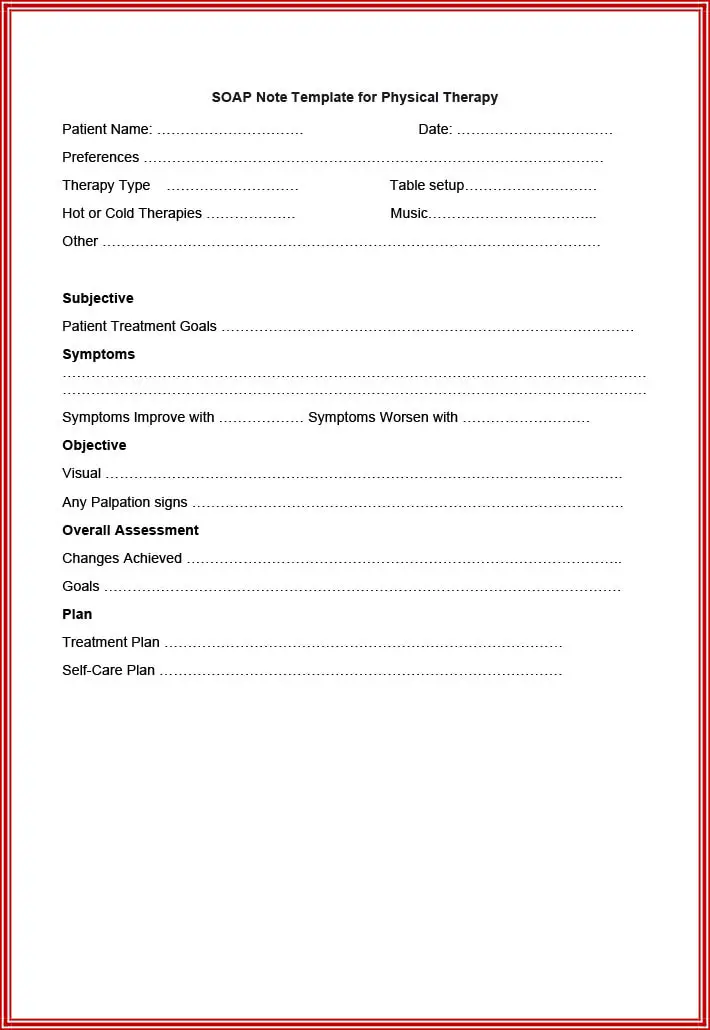
Subjective:
As you can see in the given format, this segment notes your patients’ feelings in detail. It includes their opinion on the progress, future expectations, current functionality, etc.
Additionally, it will prove beneficial to gain reports from caregivers and family members.
Objective:
This is the part where your analysis and observations come in.
You can include the equipment to be used, patient vitals and measurements, duration and frequency of the treatments, etc.
Assessment:
This information should highlight your patient’s diagnosis as it will lead the next therapist to go ahead.
Mention the recommended treatments and why you chose them to achieve specific goals, how you intend to execute them, etc.
Plan:
Your final step while writing the SOAP notes as a physical therapist is to specify the treatment outline.
Mention any modifications in your method, steps you will take in the upcoming visit, etc.
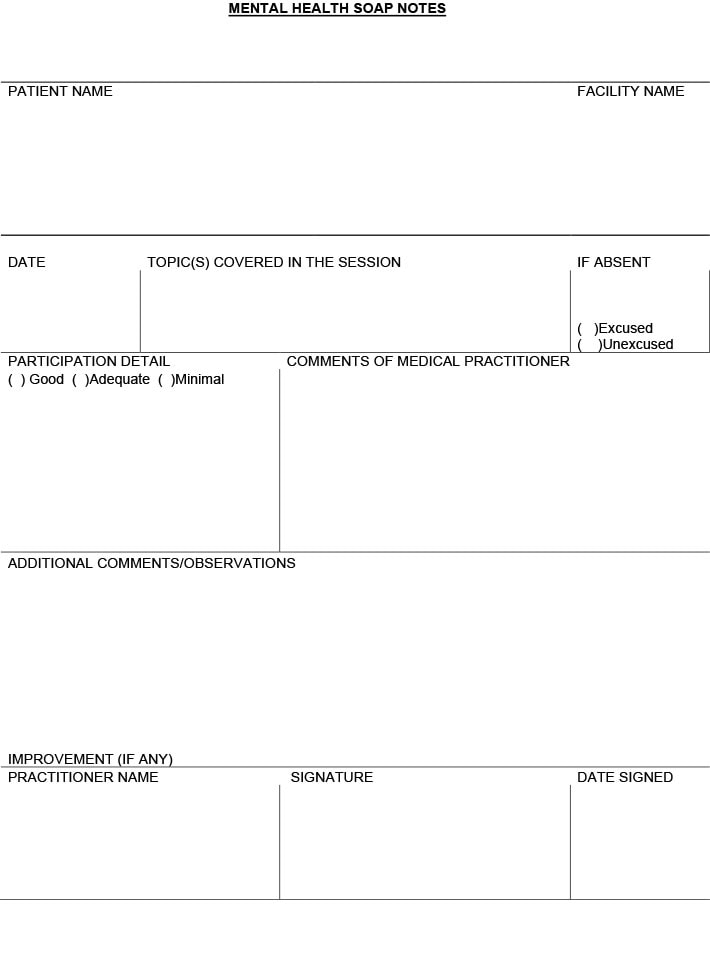
For Mental Health
Writing quality and concise SOAP notes without skipping the important records is a skill.
However, SOAP notes hold the utmost significance for a mental health professional like you for your client’s future treatment.
Here are three scenarios with the examples each for you to envision the methods through which you can use SOAP notes.
Additionally, find attached templates to download and understand the format for behavioral health care settings.
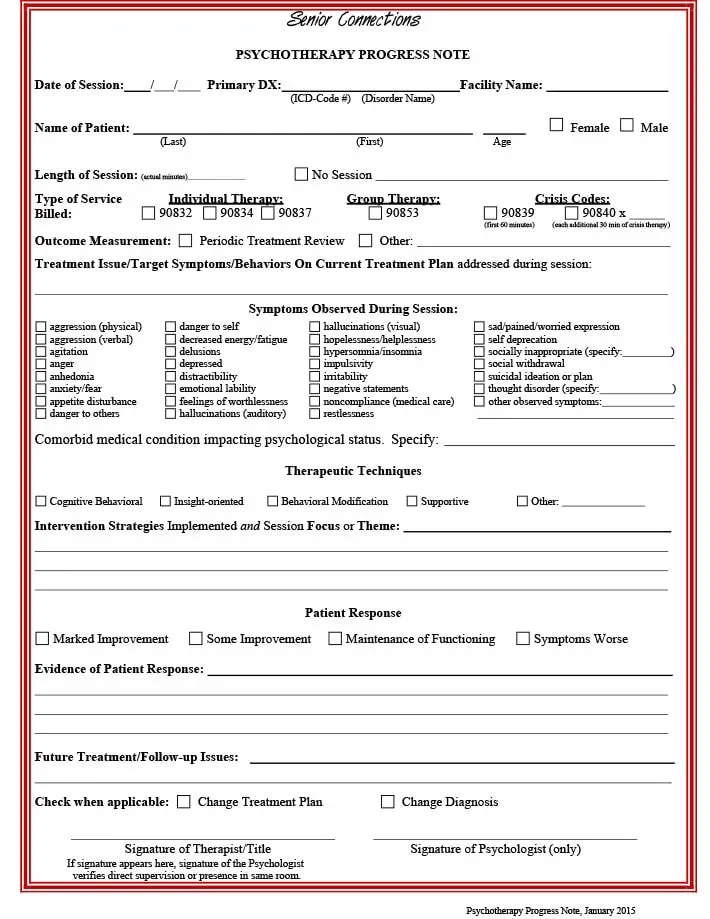
Psychiatry Format
- Subjective: State what your patient expresses about his/her general well-being, depressive symptoms, mood, etc. Ask your client and make notes on their sleeping patterns, improvements from the prescribed medication, and side effects, if any.
- Objective: Record your opinions about the improvements that you notice, prevailing behavioral condition (alert or not), any apparent emotions, etc. Also, mention lab results.
- Assessment: Any disorders or psychotic features that you note.
- Plan: The medication dosage and counseling that the client must take up in the following visit, along with modification plans.
Individual Therapy Example
- Subjective: The client’s perspective on his/her development, cravings, symptoms, or distractions, if any, general thought process, etc., stated by him/her.
- Objective: Document your observation of the client’s condition. It may include factors like calmness, signs of withdrawal (or attention), tremors, etc.
- Assessment: Overall analysis of improvement (or degradation), diagnosis, possible problems, and required treatment.
- Plan: Document your future plans and techniques that you intend to continue in the subsequent visit.
Group Therapy Example
SOAP notes for a group therapy session are relatively different from the individualized ones.
You need to be highly precise while making these SOAP notes because, in such sessions, you will have multiple patients with varying conditions.
This documentation requires you to record specific notes on individual patients in the same SOAP format.
Additionally, you need to document the type of group, session goals, information of the present members, and the head’s interventions expedited. It is a relatively time-consuming process.
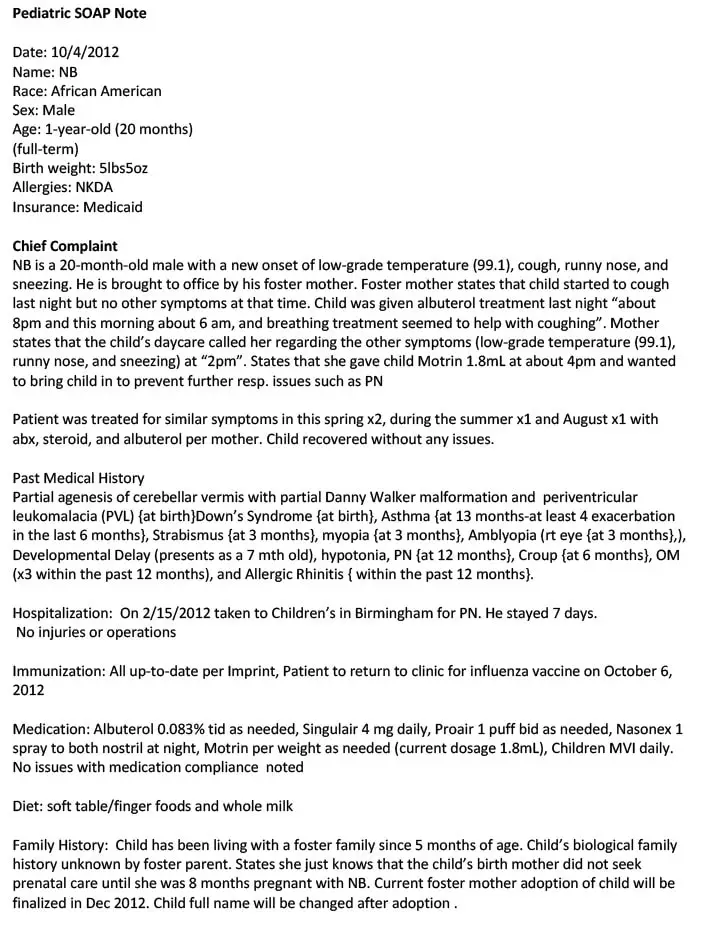
For Pediatrics
The example for pediatrics is considerably different from the other SOAP notes. That is because usually, children are not able to express their ailment comprehensively.
Therefore, as a pediatrician, you will have to make notes based on your examination and the information provided by the child’s guardian.
- Subjective: This part of SOAP notes will include everything that the patient describes his/her state. You need to document things like present health state, symptoms, when it started, any pain or wellness problems that occurred recently, past medical records, etc.
- Objective: Here, you need to document all the crucial signs and test results. These will include temperature, blood pressure, and state of the abdomen, nose, neck, chest, heart, or other relevant body parts.
- Assessment: This part of the documentation is where you need to state your analysis report and observation. Based on your examination of the patient, mention any differential diagnosis, possible problem, etc.
- Plan: Documentation of the required medicines, further tests or consultation required, when the patient should visit subsequently, etc.
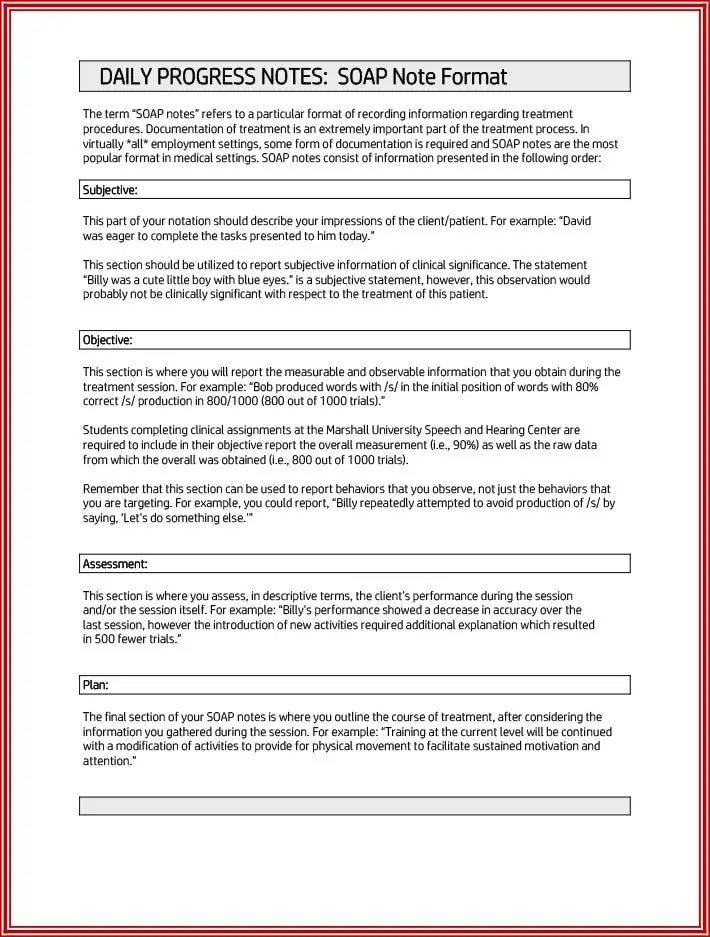
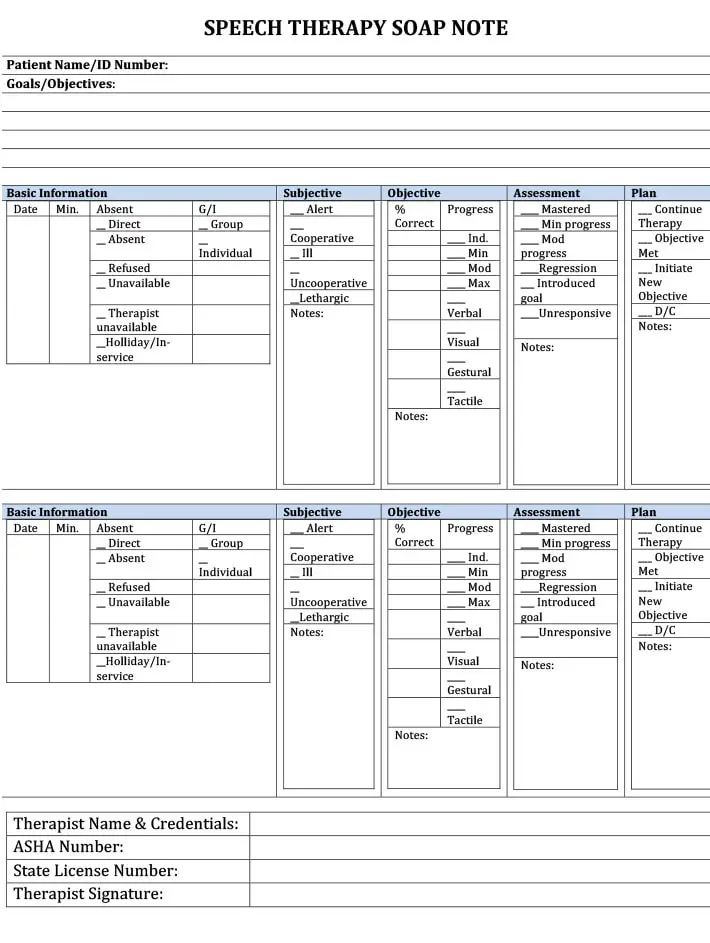
For Speech Therapy
In this example, you will learn about writing SOAP notes for a speech practice session.
Though it includes all four components of a standard SOAP document, this piece documents different information.
- Subjective: This is the patients’ report that they or their care providers communicate with you. It will include any improvement that your client noticed or if s/he has any queries regarding the session. You may ask your patient about the prevailing conditions to document in this part.
- Objective: In this part of SOAP notes, you will include your analysis of the patients. Whether you noticed development (or degradation) in their speech, their performance, or any goals they achieved. Additionally, you must mention the test scores to support your observation.
- Assessment: According to the first two components, here, you will document your client’s growth. Whether they can pronounce words, communicate without any problem, etc., clearly. You can also create this report by comparing the results with that of the previous session.
- Plan: Here, you must identify what needs to be done after this and next session. For example, if your patient cannot pronounce a few words, you must create specific treatment steps to improve this problem.
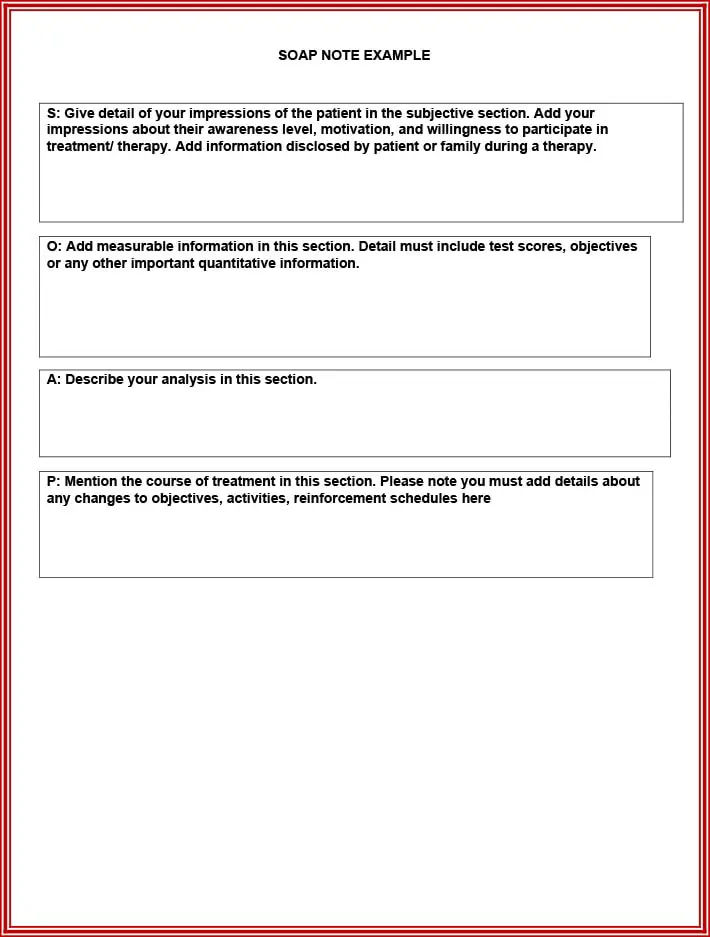
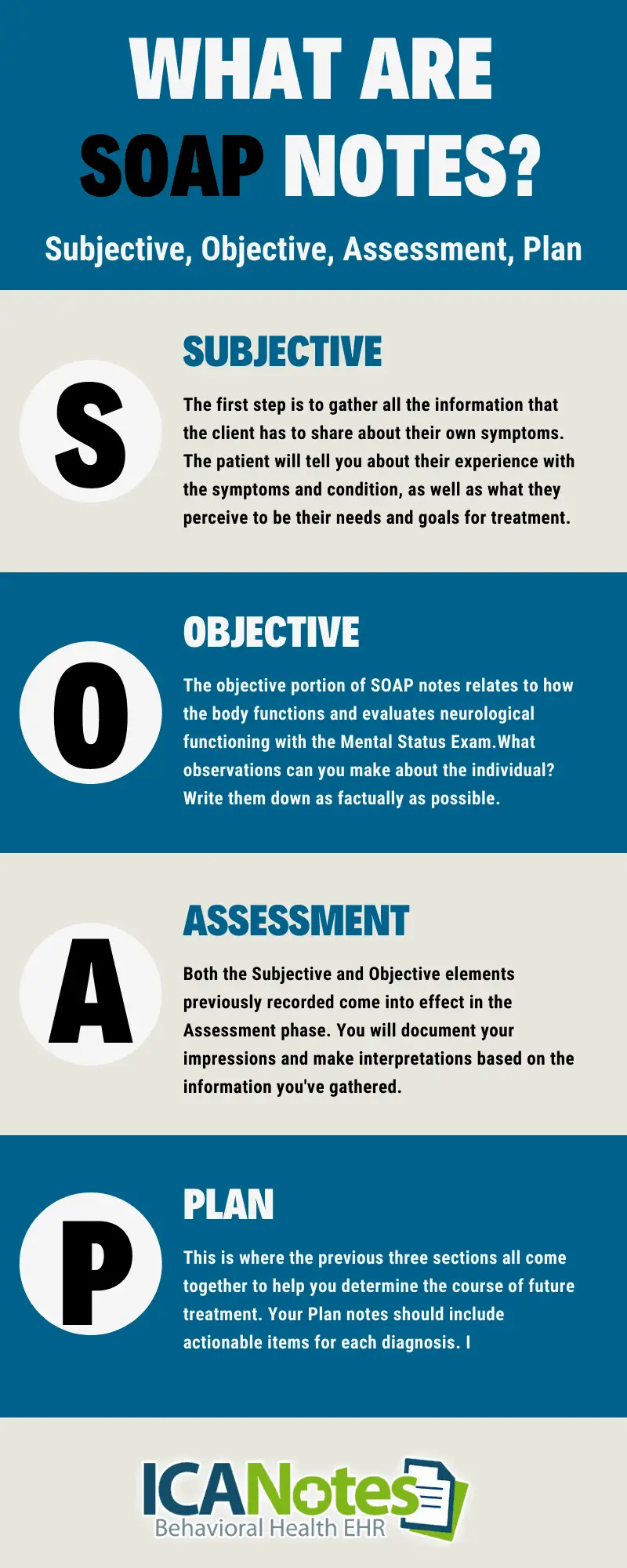
What Is A SOAP Note?
It helps record the patient’s current condition and symptoms, past medical records, medication, and other valuable details.
Primarily, it is a well-structured document used between practitioners to communicate about a particular patient’s medical state.
The concept was first invented by Doctor Lawrence Weed almost over 50 years back.
During those times, the recording and documentation of a patient’s diagnosis were rather vague, leading to confusion in the decision-making process.
Dr. Lawrence Weed researched and created an extensive Problem-Oriented Medical Record structure, with SOAP notes being a vital element.
With the introduction of the note, professionals could analyze and make decisions with concrete medical history. Moreover, it also became an easy mode of communication between different doctors and attendants of the same patient.
Today, SOAP notes are used expansively throughout the world.
They act like evidence of your skill and practice to keep as a record in the hospital.
Moreover, it is also proof of consistent and steadfast treatment for the patient’s family.
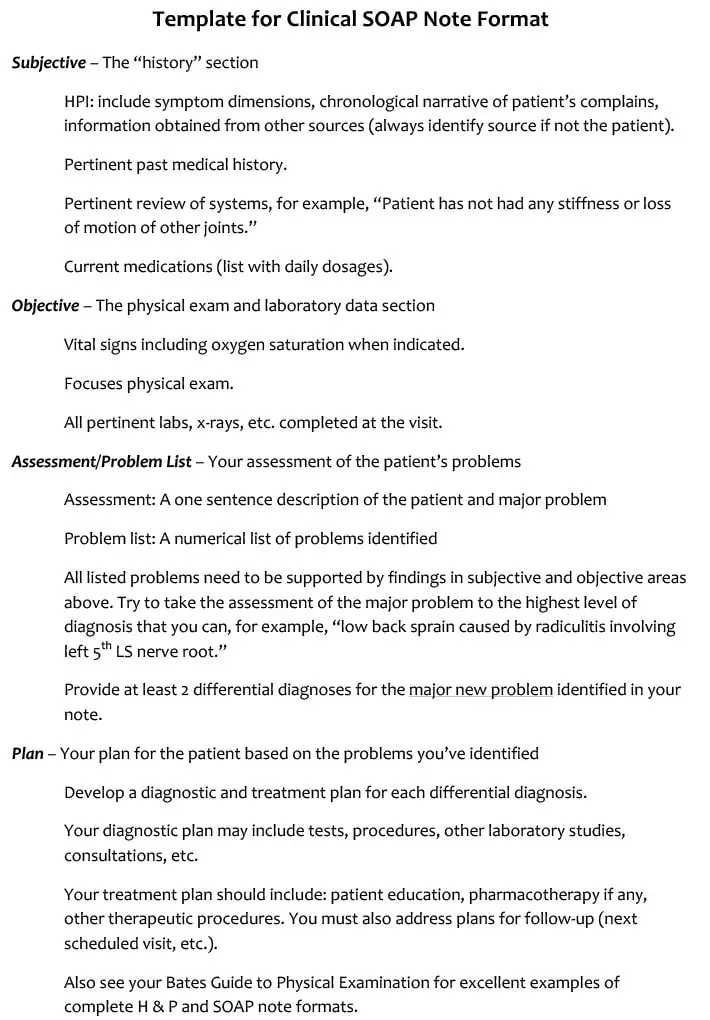
Components
It is mainly divided into 4 components, each of which holds particular significance for recording patients’ health status.
- Subjective: This section states the patient’s current symptoms and previous ailments. This component includes Key Complaint, History of Present Illness, and Details of Previous Medical Conditions.
- Objective: The objective section is essentially the result of lab tests, data, and findings. It reflects the various signs that may or may not confirm the symptoms stated in the previous section.
- Assessment: It is the part that states the medical analysis according to information in the first two sections. Here, you need to list the potential health problems and differential diagnoses (possible issues).
- Plan: This section points out the required action like medication, further consultation, or tests if any.
How To Write?
As you may have noticed in the example mentioned above, this type of documentation is pretty concise.
Although you got SOAP notes and templates for several medical field scenarios, here are tips on how to write one.
Use a SMART Template
Using a template is an excellent way of documenting patient health conditions. However, you must try to opt for a SMART (Specific, Measurable, Attainable, Relevant, Time-Based) SOAP template.
These will help you achieve your purpose of correct documentation effortlessly.
Keep It Short
The prime reason behind maintaining it is making it easy for other physicians to understand the client’s health status.
They do not have time to flip through pages, which is why you need to make short and informative notes.
Always Cross Check
You may need to take down notes in a hurry during the different sessions.
That is why you must always cross-check your notes against a template.
During this process, you can also rectify the document and ensure it has the correct information.
Right Language that is Easy to Understand
Your notes will be used by care providers, other physicians, hospital records, etc. Therefore, you must always include the right words like observed, evaluated, addresses, clarified, etc.
Remember that if it is well-structured, your SOAP notes will be easy to understand.
Mistakes To Avoid
SOAP note examples and writing tips are not enough.
You must also address the common mistakes that you need to avoid during documentation.
- Avoid judgemental narratives of the patient, and focus on a neutral perspective instead.
- Do not mention the names of family members or care providers. It may confuse the other professionals.
- You must not use an informal tone in a medical record.
- Avoid lengthy and wordy phrases.
- Never make statements based on your thoughts in the absence of factual data.
While you cannot mention information not relevant to the SOAP components, you can surely add other sub-divisions at the end.
These may include the educational background of the patients, referrals, consultation, etc.
Summing Up
These notes are necessary to record crucial patient data. Items like medical history forms and a doctor’s note help the patients and other professionals to store and share information systematically.
You can refer to the SOAP note example that you require and create one of your own with utmost ease!
References & Sources: